In Property and Casualty Insurance, Auto claims are one of the most commonly filed claims. The count typically ranges in the millions every year. They make up the majority of claims compared to other types for any insurer that provides Personal or Commercial Lines policies.
Due to the large volume of claims, insurers need to maintain a skilled and efficient workforce for various stages of the claim lifecycle. This lifecycle includes claim intake, assessment, litigation (if needed), and settlements to resolve claims in a timely manner.
Challenges to Claims Assessment
One of the most critical processes in Auto claims is assessment or evaluation of damage. Skilled material damage adjusters require highly complex tools to assess damage and to arrive at an appropriate repair estimate. In the absence of these tools (or due to lag in communication between claims administration systems and external estimation tools) claims settlement may be delayed.
Whether delays are a result of manual intervention involved in the review of estimates or in the processing of payments, they undoubtedly bring stress and frustration to customers. In addition to the inability of Claims systems to perform complex internal tasks – such as estimating auto damages and repair costs – there are a multitude of other challenges that impact the efficiency of claim adjusters, sometimes resulting in om hasty estimations and settlements. This includes:
- Limitations of legacy systems to integrate and communicate efficiently with estimating tools provided by various vendors in the industry
- Human intervention needed for the manual review of estimates and processing payments
- Human errors in estimate reviews and processing payments
- Lack of automation leading teams to be engaged in repetitive tasks on straightforward claims instead of focusing on severe claims (often involving high complexity or large payments)
Improving Claims Assessment with Straight Through Processing
Modern claims systems use built-in functions to integrate external vendor applications for various services. One of these is Material Damage Assessment. By integrating with external vendors, like repair shops to assess the claim damage, insurers can shift a critical part of the claim process to the people who will be repairing the damage and get a more exact estimate for payment.
Once the estimates are received in the claim system from the vendor application, adjusters can leverage straight through processing (STP) to automatically create checks and process payments by simply clicking a button.
Straight through processing is a functionality that allows seamless, automated payment processing in claims systems with minimal or no manual intervention. Modern core systems—such as Guidewire ClaimCenter—typically offer this capability.
The typical manual process for reviewing estimates and creating system checks requires all the relevant ”Payee” information (such as name, address, coverage, payment type, payment mode, and amount) to be verified. This process is eliminated by STP. Adjusters can use the “Payee” information already saved in the system. Payments can then be processed using the mode of payment selected by the Repair Shop (including paper check, EFT, etc.). This results in a quicker turnaround and eliminates any potential errors from repetitive tasks on straightforward claims due to human oversight.
Enhancing Straight Through Processing with Automation: One Insurer’s Journey
Although the “STP” button alleviates the manual efforts in modern claims system to a certain extent – including steps like entering all the relevant “Payee” information, the mode of payment, amount, etc. – the manual effort needed to login to the specific claim and to click on the button, is still needed.
One leading insurance carrier recognized this required effort and set out to automate this process to invest their adjuster’s time more wisely and efficiently.
For this insurer, due to the high volume of auto claims qualifying for STP – the average is about 250 claims per month, per adjuster – and any subsequent “Supplemental Estimates” received on these claims result in a significant investment of time.
The carrier needed about 35 of their impacted, experienced adjusters to focus more on other critical activities like auditing the quality of the estimates, helping the customers with their questions wherever needed, and adjudicating more complex claims.
To build automation into their STP, the insurer worked with their vendor partner to integrate with an external vendor – direct repair shops –to enter estimates and run an audit on those estimates to determine if they qualify for STP payments.
For qualified payments received in Guidewire ClaimCenter, the typical process is for the adjuster to click on the STP button and process the payment. With a complex enhancement to ClaimCenter, the system was able to determine estimates or supplements qualifying for STP. The System ran validation rules within the claims system to verify whether all the information on the claim file was both, comprehensive and valid for processing a payment. When valid, the system automatically triggered the STP process – creating checks with all the needed information, automatically.
The need for the adjusters to log in to each qualifying claim file to trigger STP was completely eliminated.
As part of the enhancement – if the validation to process an automatic payment failed, the system will trigger an Activity to the concerned adjuster. This will notify him or her of the failure and the reasons or discrepancies on the claim file. The adjuster can then fix the discrepancies on the file and mark the activity as “Complete,” which will automatically trigger the STP process again. This enhancement allowed for the processing of automatic payments.
Adjusters no longer needed to navigate through multiple screens to trigger the STP. Automated validation of the claim file prevented any potential invalid payments – ensuring quality as well as enhancing the experience of adjusters and hence the claimants.
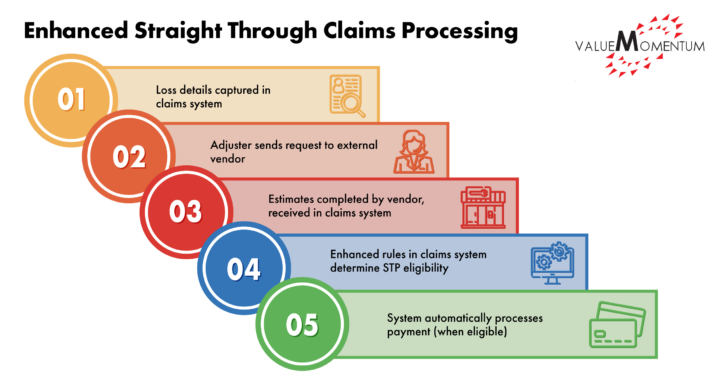
The claims assessment and payment process with enhanced STP is then simplified to these steps:
- Loss details are captured in the claims system
- The adjuster sends a request through the claims systems to an external vendor application for estimates and repairs
- Estimates are completed by the vendor and received in the claims system
- Enhanced rules in the claims system determined if the claim is eligible for Straight Through Processing.
- When eligible, the system automatically creates a check and process the payment – without the need for any manual intervention.
Leveraging Modern Technologies for better Claims Experience
Filing a claim can be the most stressful experience a customer can go through. It is a critical phase not only for the person filing the claim, but also for the insurer. Enhanced straight through processing can help leverage modern technologies and claims systems to provide an efficient and expedited claims experience to both adjusters and policyholders.
Due to automation of the repetitive manual task, enhanced STP allows adjusters to focus on more severe claims involving complex adjudication, large payments, and auditing the quality of estimates. This way teams can utilize their time more effectively. Enhanced STP also prevents potential issues caused by human error. It reduces additional efforts that might otherwise have been spent on correcting these errors.
Quick turnaround helps customers be indemnified sooner, resulting in increased customer satisfaction and a more robust insurer-insured relationship. When the experience for both claimants and employees is improved, insurers are more able to optimize the customer experience and focus on the goal of driving growth with their modern core systems.
